By Stephen Asher
In the weeks leading up to my seventieth birthday, nights were fraught with recurring, anxiety-infused dreams followed by periods of sleeplessness. Suddenly, I was old, and the luxury of extended middle-years could no longer provide shelter from age’s accumulating reminders.
But the great day passed, sleep improved, and a new vista took hold, perhaps in recognition that the bulk of life’s experience had amassed. The sharpening dialectic responsible for the formation of character was expended. In particular, these late life clarifications have served to illuminate the shaping and refining of a career in medicine. With respect to these penultimate years in a long career, it has become evident that unique distractions and moral quandaries emerged—testing some of my most basic structural tenets—which in turn have served as a catalyst for the thoughts that follow.
Medicine has seemed a calling, not a manufactured pursuit. I cannot ignore the shaping influences of, for example, my physician father, my internist uncle, and my mother, a registered nurse, whose heart was always in the arts. Her mother was also a nurse. There was, perhaps, even my great-great-grandfather, a nineteenth-century pharmacist in Mississippi. The notion of a calling implies some otherworldly attraction, but as a humanistic rationalist, I find it difficult to accede to this premise. Nonetheless, as I willingly answer late night phone calls from distant physicians, concerning patients that I will likely never see, the designation of calling often seems apropos.
In contrast to the cornucopia of college, medical school, particularly the first years, seemed an exercise in internalizing massive amounts of information, much of which was verging on obsolete.
Durable attractions to the biological and physical sciences as well as to verse and literature coexist in me. In contrast to the cornucopia of college, medical school, particularly the first years, seemed an exercise in internalizing massive amounts of information, much of which was verging on obsolete. Where were the subtle and thought-provoking professors, whose humanism was ever on display? Where were the teaching assistants who helped to smooth over the rough patches? Where were the after-hours discussions of ethical issues?
Conversely, the clinical years felt exciting and relevant, with each four- to eight-week block permitting exposure to the array of disciplines. Despite this exposure, I found it troublesome that these assumed roles seemed an imperfect fit, leading to the angst of indecision and to a recurring concern that I may have pursued the wrong path. Through the vagaries of scheduling, it was not until the final rotation of my fourth and final year that neurology was upon me. A medical internship was followed by a Public Health Service appointment, entailing research at the National Institutes of Health. Residency and academic faculty years followed, to the point of maturation and self-identification as a neurologist, suitably trained for this most cognitive discipline.
As a physician, I have had the honor of entering the life of my chosen community, as well as into the lives of many hundreds of people. The perspective gained from each has been incalculable. This perspective was abruptly reversed when, at about age fifty, I was found to have advanced intra-abdominal cancer. Definitive surgery was rendered at a tertiary medical center far distant from my home. I opted to forego offered chemotherapy and have outlived the odds; a 50 percent five-year survival rate has given new meaning to the coin toss. At that moment of my surgery, I witnessed medicine as a fragmented landscape, each participant providing care within carefully defined, perhaps protected, skillsets. Hospitalized, I encountered the despair and loneliness of the night, and I came to resent the attention of overworked nurses, many of whom, however well-intentioned, spoke English as a second language. Wherever I turned, I had to look hard to find evidence of curiosity or caring. At this moment, I realized that without the love of immediate family and the endless grace of a faithful neighbor, the experience would have verged on the unendurable. Having seen the other side of the medical coin, I resolved to do better.
The practice of medicine has weathered the introduction of forces into the decision tree that required compromise, often perverting the moral compass. These distractions and compromises, some market- and policy-driven, some as a consequence of one’s employer, often do little to benefit either medical intent or dedication to the best interests of the patient. Additionally, in sorting through complex medical issues, most seek to embrace rationality and science, supported by a framework of functional anatomy. Thus, medical decisions can be run through well-practiced filters, permitting the achievement of relatively cogent conclusions. Occasionally, assuming complete parity, the medical decision tree may result in several equally compelling arguments.
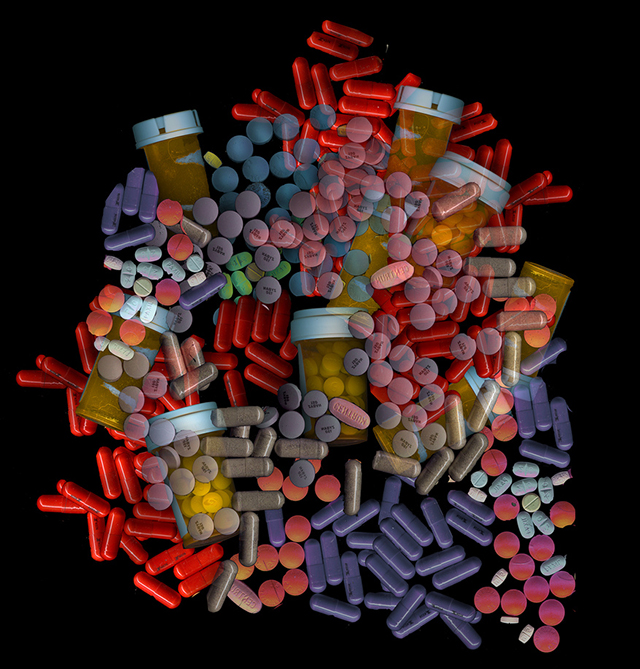
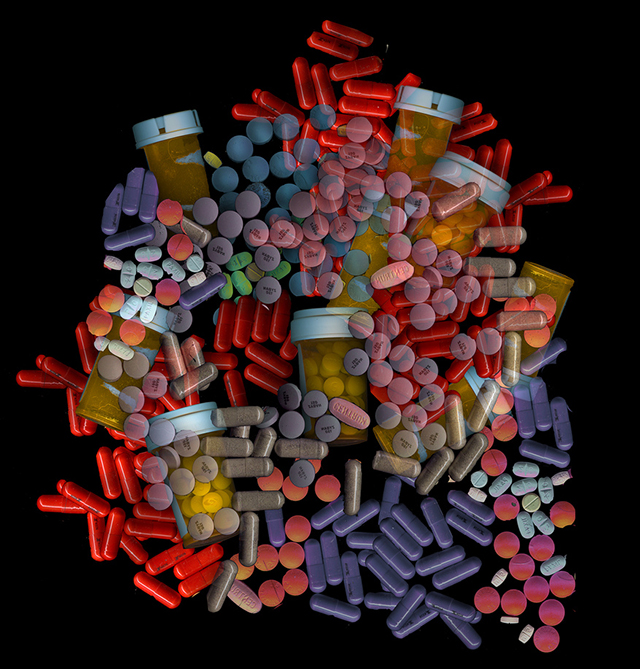
Unfortunately, the beauty of this rationality is increasingly degraded by pitfalls. In the context of medical therapeutics, several comparably effective options may coexist. As a physician, I am presented information daily, varying in scope and quality, ranging from peer-reviewed medical publications to the persuasions of the pharmaceutical sales representatives, or as presented to me by patients who have consulted with “Dr. Google.” Regarding prescribing habits, drug companies are able to purchase prescription sales information from dispensing pharmacies, presented as a function of zip code and occasionally identifying a prescribing physician. The sales representative may know who prescribes what and how often. This came as a surprise to me.
In terms of steering a patient through the structure of the medical system, there exist multiple perverse incentives. Many of them are too deeply buried to be readily visible to the patient.
Equally unsettling was that, if I wanted to opt out, I was required to make application. In other words, the default position is both comprehensive reporting and an identifiable prescriber. I exercised the opt-out because I could not see how this information was helpful to my patients. It primarily seemed like a marketing instrument, providing the sales representative with the knowledge of which physicians would be fruitful targets.
In terms of steering a patient through the structure of the medical system, there exist multiple perverse incentives. Many of them are too deeply buried to be readily visible to the patient. Some are superficial conflicts of interest. For example, the strength of a physician’s recommendation may be due to his affiliation with a drug’s maker. Does the office accept samples? Is the prescriber on a drug maker’s speakers’ bureau? Is the physician’s recommendation limited by his employer’s so-called “formulary,” a catalog of the drugs available within the system? Does he maintain an equity position such as stock ownership with a drug maker?
For a patient to be an enlightened consumer of services, an accurate understanding of real costs is essential. In reality, such costs are often obfuscated by complicated organizational influences. When a physician is employed by a health care entity, it is in his best interest to ensure that his employer, be it a hospital or multidisciplinary clinic, utilizes its own provided services. The inherent menu of internally provided options ignores costs and provides complex disincentives to refer a patient to a more cost-effective outside imaging service, clinical laboratory, or independent consultant.
Further confusion can emerge from a review of the phantasmagorical hospital bill, which is based on the hospital’s bill of fare, the so-called “chargemaster,” an entity inaccessible to physicians and patients alike. It is within this accounting device that resides the $8 aspirin and the $30,000 knee prosthesis. This chargemaster is an economic construct that allows a hospital to arrive at suitable overall charges based on the use of certain services and wares. The line items have very little to do with salary or acquisition costs.
Likewise, medication costs, often devastatingly high, are equally obscured by means independent of the chargemaster. For example, although a patient with multiple sclerosis may take comfort in a modest monthly co-payment, she is likely unaware that this sum is a miniscule offset against the $5,000-$8,000 cost per month for the latest monoclonal, paid for through insurance. These pharmacy benefits we all depend on, offered through our insurance company, are arrived at only after extensive negotiations between the insurance company’s purchasing officer and the drug maker. These bulk purchase pricings are closely kept corporate secrets.
Both patients and physicians would be so much better off with this information. If truth and transparency were applied to these negotiations, it would really not be too difficult to shine a light on these breathtaking, closely-guarded realities.
One cannot apply rational tools in the presence of such powerful distractors as these. To a great degree, the glue in this “transaction” is the trust imbued in the physician. And, to an equivalent degree, the patient’s implied trust becomes the physician’s responsibility. The physician uniquely possesses the power of the pen, controlling the flow of revenue through the labyrinth.
Becoming an effective physician has been a continuous dialectic, shaped by the dialogue of parallel themes: empiricism and wonder, science and humanity, rational skepticism and humanism. But, to carry the metaphor, in violation of geometric principle, the two vectors have gradually shed their separation and have increasingly shared their attributes. I prefer to believe that it is a consequence of the unifying properties of wisdom. Wisdom is achieved to a great degree by a commitment to the vitality of the intellect. One of several consequences of this approximation is that each passing decade has allowed me to live closer to my tenets and diminish the intrusion of unhelpful thoughts in the healing process.
Just as there is less of me, there is a more gratifying and valuable appreciation of the essence of the patient.
Perhaps this is another way to simply say that, just as there is less of me, there is a more gratifying and valuable appreciation of the essence of the patient. When possible, I make an effort to see each patient as inhabiting a point along the arc of life, contextualized to circumstance. No longer is it just an elderly, retired laborer with a painful neuropathy or a single mother with severe insomnia kiting two jobs and three children. Rather, every person lives and will live along their trajectories.
Much of the foregoing would require a young physician to possess a healthy dose of confident humanism. My hope is that the process of medical student selection would reward this attribute and that it would be an identifiable touchstone in student selection. Were humanism nurtured during the medical school years, I would offer that this perspective would remain close to the hearts of these physicians. When shared by the young and the old, that humanism allows us to ignore the burgeoning diversions and the corrosive influences, and to incorporate the essence of the patient into the rendering of the prescription.
In my pocket, I carry a touchstone, bearing the engraving “Take Medicine Back.”
This then is the prescription and we all hold the pen.