Whenever I complained of a sore throat as a child, my father would press his fingers gently behind my jawbone, checking for swollen lymph nodes. “I think you’re going to be okay,” he would say upon completing his examination. This was his verdict, too, when I called him from college, miserably ill with what he identified as “probably influenza.” I asked him if there was anything I could do and he suggested, to my disappointment, drinking plenty of fluids. Then he recommended his grandmother’s prescription for a bad cold—buttered toast dipped in warm milk. He described the way the butter floated on the surface of the milk and how comforting he found his grandmother’s care. I wanted to know if there was some sort of medicine I could take, but what I needed, my father understood, was comfort. As an adult, I still never cease to feel a little surprise when a doctor reaches behind my jawbone to check for swollen nodes. I associate the tenderness of that gesture with my father’s care.
Paternalism has fallen out of favor in medicine, just as the approach to fathering that depends on absolute authority no longer dominates parenting. But how we should care for other people remains a question. In his discussion of efforts to control childhood obesity, the philosopher Michael Merry defines paternalism as “interference with the liberty of another for the purposes of promoting some good or preventing some harm.” This type of paternalism, he notes, is reflected in traffic laws, gun control, and environmental regulations. These are limits to liberty, even if they are benevolent. Interfering with the parenting of obese children, he argues, is not necessarily benevolent. There is risk in assigning risk. Children who are already stigmatized for their body type are further targeted. And families who are identified as “at risk” for obesity become at risk to discriminatory oversight. The prevention of risk, Merry observes, is often used to justify a coercive use of power.
Doctors may be tempted to give patients what we want, even when it is not good for us.
Autonomy is usually imagined as the alternative to paternalism. But in what is sometimes called the “restaurant model” of medicine, the paternalism of doctors has been replaced by the consumerism of patients. We order tests and treatments from a menu based on our consumer research. And the doctor, who was a father in the paternalistic model, is now a waiter. The idea that the customer is always right, imported to medicine, is a dangerous dictum. “If you keep telling people it’s just a marketplace and that they’re just clients and that autonomy of the patient is what must be served to make them happy customers,” the bioethicist Arthur Caplan warns, “then you have a collapse of professionalism in the face of consumer demand.” Doctors may be tempted to give patients what we want, even when it is not good for us.
“Why does the term ‘paternalism’ have such bad press in medical circles?” asks physician John Lee. “Did everyone really have such a hard time with their dad that the reason seems self-evident?” He is paternalistic, Lee admits, but “in a good way.” A return to paternalism, good or bad, is not the only alternative to consumerism. In a response to Merry’s critique of paternalism, the educator Barbara Peterson proposes that we think of the problem of childhood obesity in terms of maternalism. Caretaking, she suggests, is not an inherent threat to liberty. “From a feminist, caring framework,” Peterson writes, “liberty is not defined as complete separation and independence from the parent.” If fathering still reminds us of oppressive control, mothering might help us imagine relationships based not just on power, but also care.
“If you’re going to get medical care,” my father says, “you’re going to have to trust someone.” I have called to ask his advice about a surgery my son’s pediatrician has recommended. My father is happy to offer his thoughts, but he is also quick to remind me that he is not a pediatrician. He does not want to be the only doctor I am willing to trust.
He is, in fact, usually the first doctor I consult. When my son woke at dawn one morning with his face so swollen from an allergic reaction that the whites of his eyes were bulging over the irises, I called my father. Did I have to go to the emergency room, I wanted to know, or could I wait until the doctor’s office opened in a couple hours? I could wait, my father assured me, and the swelling was not dangerous. “It’s just fluid,” he said. I now repeat “it’s just fluid” in my mind every time my son’s eyes swell.
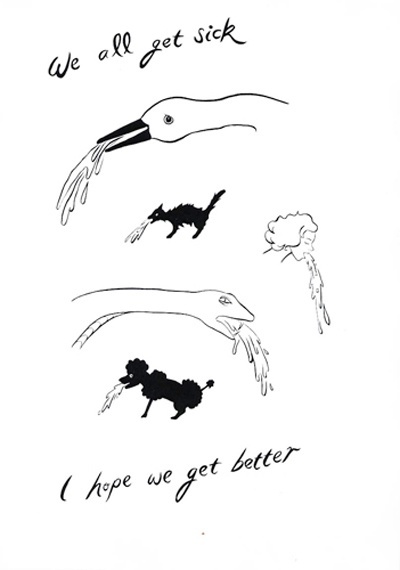
My son has unusually severe allergies, which he developed at an unusually young age. His pediatrician calls him her “outlier” because he is a statistical anomaly. By the time he turned three, his allergies had led to swelling in his nasal cavity, and this swelling had led to painful sinus infections, which we had cured with antibiotics several times, but which inevitably returned. After the third round of antibiotics, the pediatrician suggested surgery to remove his adenoids, which had swelled so much that they were completely blocking his nasal passage.
I crouched next to my son’s bed, holding my own breath during the pauses in his breathing to gauge how long he was going without air.
Surgery struck me as overkill, and I was not eager to have part of my son’s lymphatic system removed from his body. When I researched the procedure, I was disturbed to discover that it was performed widely in the early 1900s as a kind of cure-all for childhood ailments. My father was sympathetic to my concerns. He himself no longer has his tonsils because a traveling doctor removed the tonsils of all four children in his family on a single visit. This was, at the time, a standard preventive measure against rheumatic fever, which ceased after research revealed that the dangers of the surgery outweighed its benefits. As a rule, it is wise to be wary of overtreatment, my father told me. But if the alternative to surgery in my son’s case was the ongoing use of antibiotics or other drugs, surgery might be the more conservative option.
I delayed making a decision for well over six months, all the while trying everything else. A friend suggested an expensive air filter, which I bought. The allergist recommended that I keep our floors clean, a Sisyphean task, considering that microscopic allergens were constantly circulating through the air and settling on the floors. But I mopped the invisible dirt and I changed my son’s sheets and pillowcases daily. Despite his protests, I flushed his sinuses with salt water every evening. I gave him a prescription nasal spray. I fed him raw honey and nettle tea. Then his breathing, already loud, became irregular at night. I crouched next to his bed, holding my own breath during the pauses in his breathing to gauge how long he was going without air. After particularly long pauses he woke, gasping and coughing. I scheduled the surgery.
The surgeon reminded me, on the day of the surgery, not to expect dramatic or instantaneous results. She had already been over this with me, and had already warned me that my son might continue to get infections despite the surgery. I was most hopeful not that the surgery would enact a miracle, but that it would simply do no harm. It was an easy, routine surgery, she assured me. The most dangerous part was the anesthesia.
While we waited in a room full of toy stethoscopes and toy syringes, the anesthesiologist arrived and asked if I had any questions. I told him that I would like to be with my son while he was put under and while he came back to consciousness. The doctor stiffened at this suggestion. Studies had shown, he told me, that the body language and facial expressions of anxious mothers can cause children to fear surgery and resist anesthesia. It seemed there were two ways to interpret those findings, I told him—one could determine that the mother’s presence is not good for the child, or one could conclude that ensuring the confidence of the mother is essential to the well-being of the child. We began to argue in low voices, while my husband and my son applied toy bandages to each other on the other side of the room. The implication that I was a hysterical woman and a threat to my child was making me so angry that it seemed possible I might actually become hysterical. Finally, we compromised. I would be allowed to hold my son’s hand while he was put under anesthesia if I agreed to position myself so that he could not see my face.
In the operating room I talked to my son from beyond his range of vision until the anesthesia took effect. Watching the muscle tone leave his face and body was disturbing, like seeing a rehearsal of death, and I was eager to go back to the waiting room as soon as he was unconscious but the anesthesiologist called after me. “Don’t you want to give him a kiss?” he asked, to my disgust.
“He won’t remember any of this,” the anesthesiologist assured me nervously. I was busy calming my son, but I looked up just long enough to say, “I will.”
A smiley-face balloon bobbed mutely against the ceiling of the waiting room. It had been trailing us ever since my husband untied it from the stuffed pig that was given to my son by the child life specialist, who assured me that the pig could accompany my son into surgery. All the doctors were very pleased about this, even the stern surgeon. They seemed convinced that the pig would be a source of great comfort to my son.
Perhaps as a punishment intended for me, or perhaps as the result of an error or just a matter of routine, my son woke from anesthesia before I was summoned to the recovery room. I could hear him screaming “Mama! Where’s my mama?” all the way down the hallway. I knew from my own experience with surgery that the moment before anesthesia takes effect and the moment after it loses effect can seem to be the same moment—in my son’s mind I had vanished. When I reached him, he was thrashing in confused panic, trying to rip the IV line out of his body. I climbed up on the gurney to hold him and stroke his hair and keep his hands away from his IV while he wailed. “He won’t remember any of this,” the anesthesiologist assured me nervously. I was busy calming my son, but I looked up just long enough to say, “I will.”
My father suggests that the time has come for another version of Dracula in which the vampire serves as a metaphor for medicine. Because, he says, “medicine sucks the blood out of people in a lot of ways.” The cost of my son’s surgery, which was considerably more than the cost of his birth, would have made it an impossible decision for many families. I was reminded of this in the days immediately after the surgery, when my son’s breathing became easy and quiet. He slept better, he put on weight, and he stopped getting sinus infections. I now regret waiting to give him the surgery, but my husband does not. It was responsible of us, he says, to be skeptical.
Either despite or because of his training, my father is himself fairly skeptical of medicine. He once joked about the two-sentence textbook he would like to write for physicians: “Most problems will get better if left alone. Those problems that do not get better if left alone are likely to kill the patient no matter what you do.” This is as much an argument for preventive medicine as it is a sigh of defeat.
Excerpt from On Immunity: An Inoculation © 2014 by Eula Biss. This excerpt appears with the permission of the author and Graywolf Press.